Sail For Epilepsy, Part 2: An Overview of Syndromic and Monogenic Non-syndromic Epilepsies
Emily Walsh Martin, PhD - May 12, 2022
Check back to our blog every week to learn more about Dr. Walsh Martin's journey and the emerging gene therapy efforts in syndromic and monogenic epilepsies.
 The medical field has come to appreciate that epilepsy is not a monolith disease, but rather a collection of disorders caused by a range of factors like genes, trauma, vascular abnormalities, and infections. These disorders present with abnormal brain activity resulting in confusion, uncontrollable movement, and loss of consciousness, among other symptoms. Seizures are categorized1 into focal and generalized based on where the abnormal activity occurs in the brain. However, the causal underpinnings of this abnormal activity are diverse and continue to be elaborated upon.
The medical field has come to appreciate that epilepsy is not a monolith disease, but rather a collection of disorders caused by a range of factors like genes, trauma, vascular abnormalities, and infections. These disorders present with abnormal brain activity resulting in confusion, uncontrollable movement, and loss of consciousness, among other symptoms. Seizures are categorized1 into focal and generalized based on where the abnormal activity occurs in the brain. However, the causal underpinnings of this abnormal activity are diverse and continue to be elaborated upon.
In some cases of genetic epilepsy, a single gene is dysfunctional. These “monogenic” epilepsies can be categorized into 1) syndromic epilepsy, which means that patients have epilepsy alongside other neurological and systemic symptoms, and 2) non-syndromic epilepsy, which means that patients do not seem to have other neurologic or systemic issues resulting from the gene dysfunction. In both types of monogenic epilepsy, advances in gene therapy transduction in the central nervous system have given rise to the use of adeno-associated virus (AAV) and other vectors to introduce copies of the functional gene to correct for the missing or aberrant genes. However, these efforts are at early stages, and so far, we still await definitive clinical data that seizures can be ameliorated in patients with monogenic epilepsy.
Below, we discuss the current efforts in more detail for syndromic and non-syndromic monogenic epilepsy. In future blogs, we will dive deeper into this topic and also discuss the considerations for patients who may choose to participate in clinical trials for these therapies.
Syndromic Epilepsies
Owing to their monogenic nature, gene therapy approaches to treating lysosomal storage diseases (LSDs) have long been pursued by the field. Collectively, these diseases are characterized by the accumulation of specific material (or “substrates”) within a specific part of the cell known as the “lysosome.” This lysosomal accumulation is due to specific defects in the genetic code of enzymes responsible for breaking down the substrates. Substrate accumulation in the cells results in organ level dysfunctions which differ depending on the gene involved and the cells in which that gene functions. However, a commonality to many of these disorders is neurological dysfunction which can present as neurodegeneration and in some cases, epilepsy2. Enzyme replacement therapy (ERT) for LSDs is unable to address the central nervous system (CNS) presentation as the therapeutic protein is not able to cross the blood brain barrier (BBB) for access to the brain. Moreover, when these disorders present with epilepsy, the seizures are often unresponsive to standard small molecule anti-seizure medicines. Indeed, almost a third of all people with epilepsy are not fully controlled by currently available medications3 and this appears to be even more common for individuals with syndromic epilepsy. Thus, new approaches to address seizures and other neurological aspects of LSDs are very much needed.
A quick search of ClinicalTrials.gov for “gene therapy,” “seizure,” and other relevant terms reveals a growing number of clinical efforts from companies and academic groups to use gene replacement therapies to treat these syndromes that have seizures as a key feature of the disease for many patients. Beyond those active clinical trials, a number of other efforts are advancing preclinically based on publicly disclosed efforts on company websites as well. These programs include efforts in the following indications which include seizures as part of their presentation:
-
Neuronal ceroid lipofuscinoses/Batten diseases (CLN1, CLN2, CLN3, CLN5, CLN6, CLN7)
-
Mucopolysaccharidoses (MPS I, MPS II, MPS IIIA, MPS IIIB)
-
Gangliosidoses (GM1, GM2)
-
Glycogen storage disease type II (Pompe)
-
Leukodystrophies (MLD, CALD, Canavan, Krabbe)
Beyond these LSD syndromes, a number of additional neurodevelopment syndromes include seizure in their presentation. Some of the diseases being pursued with gene therapy efforts in this category include:
-
Neurodevelopment disorders (Rett, Dravet, CMT1A, Angelman, Niemann-Pick, CDKL5 deficiency disorder)
In both LSD and neurodevelopment categories, the therapeutic concept is straightforward: replace the defective enzyme in as many cells of the body as possible. Then, this corrected enzyme should act to clear the harmful accumulated substrates from the lysosomes. Moreover, as it is unlikely that 100% of cells will be directly corrected by the therapy, the hypothesis is that for those genes where the product is secreted, the gene therapy may “cross-correct” and benefit neighboring cells which were not themselves corrected.
However, a key open question for all of these diseases is whether gene replacement after symptom onset for the disorder can address the frequency or severity of seizures that patients experience. And moreover, if treatment is shown to be effective in one of these disorders, would that benefit translate to success in other disorders caused by different genetic defects?
The hope is that in coming years the readout from ongoing clinical trials will shed light not only on the benefit of gene replacement for neurodegenerative aspects of many of these disorders but also on its impact on seizures. It remains to be seen whether current gene therapy approaches will correct enough cells to be beneficial for these disease endpoints or whether novel capsids or administration approaches with improved ability to correct a greater number of cells in key tissues will be required to have the maximum benefit to patients.
Non-syndromic Monogenic Epilepsies
In addition to the efforts described above for syndromic disorders where seizures are one component of the disease presentation, recent efforts have revealed that perhaps 1-2% of patients with non-syndromic epilepsy are due to a monogenic mutation.4 Preclinical programs pursuing these gene targets are beginning to emerge including publicly disclosed efforts for SLC6A1, SLC13A5, Lafora disease (EPM2A or EMP2B), and KCNQ2. Additionally, there is at least one effort to explore a gene augmentation approach in epilepsy by delivering Neuropeptide Y5 as well as its receptor (Y2) in a number of drug-resistant epilepsies.
Unlike the syndromic epilepsies where gene correction often needs to occur both in the CNS and systemically, it is expected that the gene replacement efforts in the non-syndromic epilepsy will focus on correcting these genes in the central nervous system through targeted administration either intrathecally or intracerebrally. However, as some of the mutations appear to act in a “dominant” fashion, correction may require a two-pronged approach of introducing a functional copy of the gene and also downregulating the mutant copy in order to generate a therapeutic benefit. Similar to the syndromic efforts above, it remains to be seen whether once a seizure condition initiates, if the correction of the dysfunctional gene can reduce the frequency or severity of the seizures.
Next Up on the Blog
Efforts to develop gene therapies to treat syndromic and non-syndromic monogenic epilepsies are actively being pursued by a number of companies and institutions. However, to better understand the potential of these therapies we need to understand what they are trying to achieve in the first place. In the next blog post, we will try to unpack how a gene therapy might function to address unmet need in monogenic epilepsies.
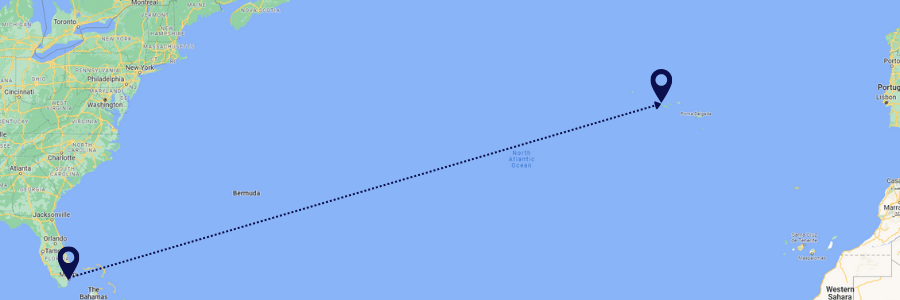
Emily Walsh Martin is a volunteer crew member for Sail For Epilepsy’s Atlantic crossing on the vessel Ingwe. When she’s not sailing, she is a consultant for gene and cell therapy companies and investors who are seeking to advance novel therapies in the clinic.
Read Part 1 here.
1. For more information about the types of seizures from Captain Phil find his blog at https://www.sailforepilepsy.org/2020/12/02/many-types-of-seizures/
2. https://www.sciencedirect.com/science/article/pii/S1096719217305024; https://linkinghub.elsevier.com/retrieve/pii/S0887899497000775; https://www.sciencedirect.com/science/article/pii/S2214426920301221; https://content.iospress.com/download/journal-of-pediatric-epilepsy/pep14093?id=journal-of-pediatric-epilepsy%2Fpep14093; https://n.neurology.org/content/90/15_Supplement/P6.267
3. For an additional overview of anti-seizure medicines from Captain Phil, check out his blog https://www.sailforepilepsy.org/2021/03/04/finding-a-reliable-mechanic-and-the-right-tool-to-fix-your-brain/
4. https://practicalneurology.com/articles/2019-oct/genetic-mechanisms-of-epilepsy