Gene therapy is a way to treat or prevent a specific disease using genetic material. One common way that researchers have found to accomplish this is by using a vector. Vectors are essentially vehicles designed to deliver therapeutic genetic material, such as a working gene, directly into a cell. There are four main types of viral vectors (adeno-associated viral, adenoviral, lentiviral, retroviral) each with their own unique characteristics, uses, and limitations.
Using Viruses
Vectors are typically derived from viruses, because viruses have proven to be very efficient at finding their way into cells. In order to make vectors safe to use, all of the viral genes are removed, and the vector is modified to deliver only therapeutic genes. The choice of which viruses to use as vectors is based on three criteria:
- How well researchers understand the virus
- How well the virus can target certain cell types
- How safe the virus is to use
 Vectors make use of the shell of the virus, also known as the capsid, to help transport working genes to the target cell. Think of vectors like envelopes being used to deliver a specific message. The envelope allows the message to be delivered, while the message inside provides new instructions to the cell on how to function properly. It might sound backward to use a virus to treat a disease, but the use of vectors is backed by years of research and has been shown to be safe, which is always a top priority.
Vectors make use of the shell of the virus, also known as the capsid, to help transport working genes to the target cell. Think of vectors like envelopes being used to deliver a specific message. The envelope allows the message to be delivered, while the message inside provides new instructions to the cell on how to function properly. It might sound backward to use a virus to treat a disease, but the use of vectors is backed by years of research and has been shown to be safe, which is always a top priority.
Gene therapy using viral vectors does more than just treat symptoms. Vectors, with the genetic information they carry, can directly target the cause of a disease and change the way a cell functions. In addition, they typically only need to be administered once and are commonly used for rare inherited diseases that have few to no other treatment options available.
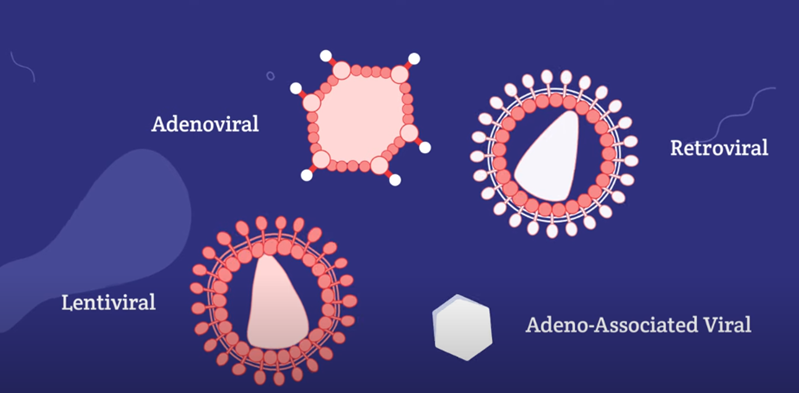
Adeno-Associated Viral (AAV) Vectors
Adeno-associated viral vectors, also known as AAVs, are typically used to deliver smaller DNA packages or genes. The size capacity of this vector may be a factor to determine which rare diseases it can target. They’re known to be safe and efficient when used for in vivo gene therapy approaches. In vivo therapy involves injecting a gene therapy into specific parts of the body so that new genetic instructions can be delivered directly to the cells within the body.
AAVs are usually non-integrating. That means the DNA they carry doesn’t typically insert itself into the cell’s genome. So, if the vector is taken up by a cell that divides, the therapeutic gene won’t be copied with each cell division and may be lost over time, thereby diluting the treatment effect. Because of this, AAVs are commonly used to target non-dividing cells, such as cells in the liver, nervous system, eyes, and skeletal muscles. AAVs can persist in patients for a prolonged period of time—possibly even a lifetime.
Innate immunity is one limitation of AAVs since many people may have had prior exposure to AAVs through natural infections. This means that pre-existing antibodies can disqualify anywhere from 30 to 70 percent of patients from clinical trial participation depending on the type of AAV being used. For these patients, their immune system may attack or destroy the vector before it can deliver its therapeutic package, rendering it useless. In addition, patients will often be limited to a single administration of therapy because they may develop antibodies following the first administration. Testing for innate immunity is becoming more widespread and is used as an exclusion criteria for clinical trial eligibility. For now, scientists are working on a variety of strategies to help combat this challenge such as creating synthetic capsids that would not be attacked by the immune system or by utilizing an enzyme that can split through the antibodies in the short term. These solutions come from knowing there is a short window of time (hours) where the vector is injected and then travels to the target cell and once the vector makes it inside the cell it is protected from antibodies.
Adenoviral Vectors
In some ways, adenoviral vectors are similar to AAV vectors. For instance, they’re most often used to deliver DNA packages into non-dividing cells. However, adenoviral vectors are larger and capable of delivering genetic packages almost eight times the size of AAVs. Adenoviral vectors can cause strong immune responses, which result in potentially harmful inflammation throughout the body and decreased effectiveness of the therapy. In recent years, scientists have worked to develop adenoviral vectors that result in milder immune responses in order to deliver larger packages with less risk.
Lentiviral and Retroviral Vectors
Lentiviral and retroviral vectors can carry larger genetic packages of RNA, which is converted into DNA. During this process, the vectors integrate into the genome of the target cell, unlike AAVs and adenoviral vectors.
The ability to integrate into the cell genome makes lentiviral and retroviral vectors best suited for dividing cells, which are targets of an ex vivo treatment approach. For example, these vectors are used to target T cells, which are a type of immune cell, and stem cells, which are special cells that can develop into many cell types. In contrast to in vivo treatments, ex vivo treatment of cells occurs outside the body. Cells are removed from the body and are cultured on plates allowing them to replicate and expand. Then these cells are treated with vectors and modified with new genetic instructions, such as a working gene. The modified cells are then returned to the body. After that, the treated cells begin to divide and generate new cells. Thanks to integration, the new genetic material is copied into all the new cells and continues to function beyond the original cell.
Other Limitations
Gene therapy using viral vectors carries a lot of potential, but is not without some risk. These examples are are in addition to limitations that have been discussed above including innate immunity and strong immune responses.
Off-target effects are when tissues other than the main target tissue may be affected after administration. Vectors that insert their genetic package into the host genome can potentially integrate at an incorrect location of the genome and cause unintended consequences. In order to maintain as much control over the process as possible, researchers have developed targeting techniques. In addition, they have the ability to monitor the vector’s long-term effects in patients at the insertion site.
Manufacturing is another challenge that is being addressed by professionals in the field. Creating a very large quantity of safe viral vectors requires time, effort, and resources. The complexities of the process add to manufacturing costs and makes it hard to effectively streamline production. Researchers will continue working towards more efficient production methods as more gene therapies are researched and approved for use.
Non-Viral Vectors
Researchers are also developing more non-viral vectors to address (or eliminate) these limitations. Non-viral vectors are cheaper to manufacture than their viral counterparts. They can potentially deliver larger genetic packages, allow for repeated dosing, and make quality control easier. Non-viral vectors also have the benefit of a lowered chance of triggering adverse immune responses.
While non-viral vectors hold a lot of promise, scientists simply have less experience with them. Many of the non-viral mechanisms are developing rapidly but challenges still remain, such as carrying capacity and ability to target specific organs or tissues. For now, they can’t be used for in vivo approaches that are common with AAVs and adenoviral vectors.
Gene Therapy and Oncology
The approach to gene therapy is very different when it comes to oncology and cancer treatment. Current vectors cannot treat 100% of cells, so gene addition or specific gene targeting strategies, which are methods used for rare diseases such as adding a working gene, simply aren’t as effective for cancer treatment. However, there are strategies that use gene therapy to treat cancer by enhancing the immune response to cancer cells. These methods vary greatly from rare disease treatment, in which a working gene sits next to a faulty gene. One way to treat cancer is to provide dividing immune cells with new genetic instructions that can turn them into cells that recognize and kill cancer cells. Another approach is to use vectors that can only multiply rapidly in tumor cells. From there, the vectors with specific instructions to kill those cancer cells are able to do so.