Mucopolysaccharidoses (MPS) are a group of genetic disorders that affect our body’s ability to break down and recycle sugar molecules called glycosaminoglycans, or GAGs, leading to buildup and causing severe symptoms. Gene therapy targets the root cause of disease and therefore may offer hope for slowing or halting the progression of some MPS disorders.
MPS and Gene Therapy
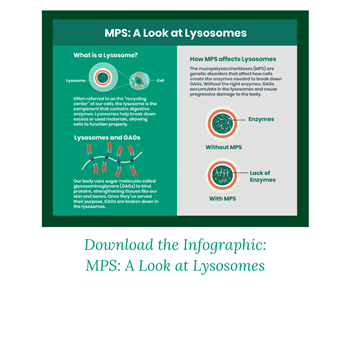
 There are seven different types of MPS, each caused by a different faulty gene. Gene therapy may be able to slow the progression of the MPS disorders I, II, III and VI, although it cannot reverse damage the disease has already caused. You may have heard that MPS I is also known as Hurler syndrome, while MPS II is referred to as Hunter syndrome and MPS III is called Sanfilippo syndrome. The faulty genes that cause the disorders affect how our bodies produce enzymes that break down GAGs. The GAGs are sugar macromolecules found in a variety of tissues, including our skin, bones, cartilage, and brain. Macromolecules are larger molecules, built from smaller organic molecules. Normally, our body naturally breaks down GAGs as part of an ongoing internal recycling process. This process occurs in small compartments of our cells called lysosomes, which help our body remove or recycle waste—including GAGs. However, without the necessary enzymes to break them down, GAGs build up in lysosomes and limit how cells function. This causes progressive damage to the body in a variety of ways, including heart disease, short stature, difficulty breathing and brain deterioration.
There are seven different types of MPS, each caused by a different faulty gene. Gene therapy may be able to slow the progression of the MPS disorders I, II, III and VI, although it cannot reverse damage the disease has already caused. You may have heard that MPS I is also known as Hurler syndrome, while MPS II is referred to as Hunter syndrome and MPS III is called Sanfilippo syndrome. The faulty genes that cause the disorders affect how our bodies produce enzymes that break down GAGs. The GAGs are sugar macromolecules found in a variety of tissues, including our skin, bones, cartilage, and brain. Macromolecules are larger molecules, built from smaller organic molecules. Normally, our body naturally breaks down GAGs as part of an ongoing internal recycling process. This process occurs in small compartments of our cells called lysosomes, which help our body remove or recycle waste—including GAGs. However, without the necessary enzymes to break them down, GAGs build up in lysosomes and limit how cells function. This causes progressive damage to the body in a variety of ways, including heart disease, short stature, difficulty breathing and brain deterioration.
 Gene therapy introduces a working version of a gene into the cells in charge of creating key proteins or enzymes. These genetic instructions are delivered to the cells using a vector, or vehicle, which are often derived from viruses. Typically, viruses are used as vectors because they are capable of entering cells to deliver genetic material. Don’t worry. All viral genes are removed and the vector is modified to only deliver therapeutic genes to cells. With the right genetic instructions, cells can then produce functional enzymes that help break down further buildup of GAGs.
Gene therapy introduces a working version of a gene into the cells in charge of creating key proteins or enzymes. These genetic instructions are delivered to the cells using a vector, or vehicle, which are often derived from viruses. Typically, viruses are used as vectors because they are capable of entering cells to deliver genetic material. Don’t worry. All viral genes are removed and the vector is modified to only deliver therapeutic genes to cells. With the right genetic instructions, cells can then produce functional enzymes that help break down further buildup of GAGs.
Depending on the type of MPS and the tissues most affected by the disease, vectors may be delivered directly to the central nervous system through injections to the brain or spinal cord. They can also be injected directly to the liver, or administered through an IV directly into the bloodstream. Gene therapy is intended to be a one-time procedure. This is an alternative to existing treatments like enzyme replacement therapy, which require lifelong administration to manage symptoms.
Pathway to Treatment
Treatment Pipeline
Investigational gene and cell therapies for MPS are being researched by Abeona Therapeutics (MPS III A and B), Lysogene (MPS III A and B), Magenta Therapeutics (MPS I), Orchard Therapeutics (MPS III A and B), and RegenXBio (MPS I, MPS II). To learn more about all active and recruiting gene and cell therapy clinical trials in the US, visit the ASGCT Clinical Trials Finder and search for mucopolysaccharidoses in the ‘diagnosis’ field.
Gene Editing and MPS
Researchers are also exploring approaches for MPS using gene editing to correct enzyme production. The goal of gene editing is to remove, disrupt, or correct faulty elements of DNA within the gene rather than to introduce a functioning gene as gene replacement therapy would, as described above. Gene editing uses systems that are highly precise to make this change to specific pieces of DNA inside the cell. There are no approved gene editing treatments yet, but there are some currently being researched in clinical trials.
Eligibility
You may be curious how people with MPS can participate in clinical trials for gene therapy. These trials offer an opportunity to receive an investigational treatment at no cost, while also benefiting the medical community and others who have the disease. Eligibility, risks, and benefits should be discussed with the individual’s disease specialist or primary provider.
To participate in a clinical trial, the individual must meet strict eligibility criteria, such as age, gender, and treatment history. A key barrier can be the time of diagnosis. Often times, people are diagnosed with MPS later in life. At that point, years and years of GAG buildup within the body may have caused irreparable damage to certain tissues and organs that gene therapy cannot repair at this time. If a patient is diagnosed at a young age, gene therapy could stop GAG buildup early on. The goal is continue research and clinical development in hopes of expanding the scope of MPS that is treatable through gene therapy.
Get Involved
Getting involved with patient advocacy organizations is a great way to connect with other families and patients affected by MPS disorders, gather useful resources, and advocate for research. The diseases may be rare, but you're not alone.