Could Gene and Cell Therapy be the Future of Endometriosis Treatment?
Eoghan J. Mulholland, Ph.D. - March 20, 2020
Advances in gene and cell therapies are rapidly evolving, so we also want to look into the great potential these therapies may have in the battle against endometriosis.
Since the month of March is Endometriosis Awareness Month, we want to explain this deliberating disease and its symptoms in order to increase understanding of it. Advances in gene and cell therapies are rapidly evolving, so we also want to look into the great potential these therapies may have in the battle against endometriosis.
What is endometriosis, and how many women are affected?
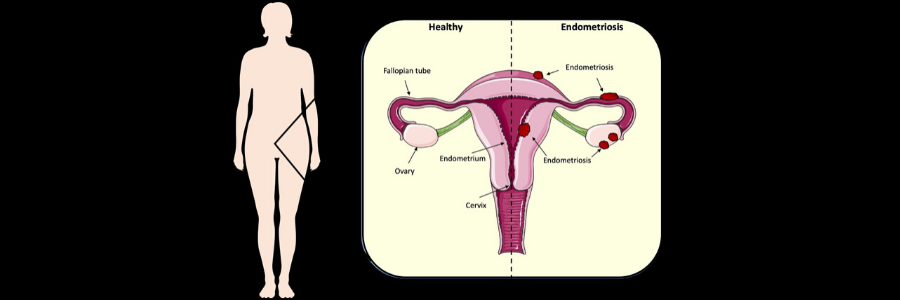
Endometriosis occurs when the lining of the uterus (known as the endometrium) grows ectopically within the body. Typically, this abnormal endometrial tissue settles in areas such as the lining of the womb, fallopian tubes, ovaries, bladder, bowels, or pelvis. In extreme cases the tissue has even been located in the lungs of patients. As with normal endometrial tissue, ectopic endometrial tissue breaks down but cannot be processed and disposed of in the same way, which leads to inflammation, cysts, excruciating cramps, scar tissue formation, and even compromised fertility.
In the U.S., it is estimated that endometriosis may affect more than 11% of women within reproductive age. Similar occurrences were true for women in the U.K., with 1 in 10 thought to have the disease. On a global scale it is estimated that there may be 176 million women who suffer from endometriosis.
Early diagnosis and treatment intervention are key to reducing patient pain and to de-risk long-term complications as much as possible. Shockingly, in the U.K., it takes seven and a half years on average to get endometriosis diagnosed.
Knowledge and awareness, therefore, is key to tackling this beast. According to the Mayo Clinic the following are common signs and symptoms to be on the lookout for:
- Painful periods
- Pain during or after intercourse
- Painful bowel movements and/or urination
- Excessive bleeding during or between menstrual cycles
- Infertility
- Fatigue
- Bloating
- Nausea
Current treatments
There currently is no cure for endometriosis, but several measures can be taken to circumvent the symptoms as much as possible. Common drug treatments include:
- Over-the-counter pain medications such as NSAIDs like ibuprofen are commonly used, but can be ineffective in many cases.
- Supplemented hormone therapy can in some cases relieve pain and inhibit disease progression. By regulating the body’s hormone levels, it stops hormonal fluctuation which leads to pain.
- Hormone-based contraceptives can be an effective therapy. They work by decreasing fertility via prevention of endometrial tissue build-up.
Alternatively, many patients resort to surgical intervention to help relieve pain or if hormonal therapies are not effective. Several surgical options exist:
- Conservative surgery aims to remove endometrial tissue laparoscopically while retaining the patient’s reproductive organs.
- Hysterectomy is often considered a last-resort for patients when other therapies are not working. This procedure is rarely recommended as it is not guaranteed to work.
Encouragingly, there is a strong research community focused on developing new treatments for endometriosis. According to www.clinicaltrial.gov, there are currently 435 trials involving endometriosis.
The potential impact of gene and cell therapy research
Gene and cell therapies are an exciting option with great potential to explore and develop personalized medicine for the treatment of endometriosis. Presently, in the aforementioned 435 clinical trials, only one of these involves a gene therapy option. More promisingly, there are currently 11 trials which involve cell therapy.
I spoke with Hugh Taylor, M.D., of the department of obstetrics, gynecology and reproductive sciences at Yale School of Medicine. Dr. Taylor et al. recently published a fascinating paper entitled microRNA Let-7b/ A Novel Treatment for Endometriosis in the Journal of Cellular and Molecular Medicine. Dr. Taylor gave the following promising statement:
“For too long endometriosis has been treated exclusively with hormones rather than targeted therapy. As we identify the molecular alterations in this disease, we are able to bring a precision medicine approach to endometriosis. Recently we have identified several microRNAs that are aberrantly expressed in endometriosis. These have served as a non-invasive biomarker of disease as well as therapeutic targets. In mouse models we have demonstrated that treatment with microRNA or their inhibitors can treat endometriosis. Gene and RNA based therapies are the future of endometriosis treatment.”
This research group had previously demonstrated that let-7b was downregulated in endometriosis, and that this reduction in expression contributed morbid physiology of the disease. In mouse models of endometriosis, the authors found that treatment with a mimic of microRNA Let-7b resulted in a significantly lessened histologic endometriosis tissue area compared to control groups (P=0.03). This cutting-edge research could pave the way for future gene therapy options for endometriosis with fantastic potential.
Cell therapy is another modality which is gaining momentum in the race for novel endometriosis treatments. I spoke with professor Serdar Bulun, M.D., who is the chair of the department of obstetrics and gynecology at Northwestern University, and he had the following to share:
“Endometriosis harbors widespread epigenetic and genetic defects. Targeting all of these distinct defects using drugs is extremely difficult if not impossible. Therefore, I predict that cell-based therapies will play a major role in the effective treatment modalities of endometriosis developed in the future. One potential treatment is the use of human induced pluripotent cells that are differentiated in vitro to healthy endometrial stromal cells.”
This highlights the monumental genetic barriers which hinder the effective treatment of endometriosis. Professor Bulun et al. have published an excellent paper entitled Generation of Progesterone-Responsive Endometrial Stromal Fibroblasts from Human Induced Pluripotent Stem Cells: Role of the WNT/CTNNB1 Pathway in Stem Cell Reports.The authors detail that the replacement of faulty endometrial stromal fibroblast (EMSFs) has potential as a novel therapy for endometrial diseases. One such route is the use of induced pluripotent stem cells (iPSCs); however, the mechanism of these cells differentiating into endometrial stromal cells is not fully defined. This paper demonstrates the successful differentiation of iPSCs into EMSFs and found that activation of CTNNB1 was critical for the expression of progesterone receptor which facilitates the final differentiation process of EMSFs before implantation .
What’s next?
It is clear that there is a still a lot to do to raise awareness of endometriosis, and also to unfold the genetic and molecular mechanisms involved in this disease initiation and development. More needs to be done to pinpoint the symptoms early and better treat the individuals who are diagnosed. The current drug and surgical options available have varying efficacy, and more action needs to be taken as no cure is available. Gene and cell therapy offers hope in this regard, given the complex architecture and genetic construction of this disease.
Dr. Mulholland is a postdoctoral research scientist in cancer genetics at the University of Oxford and a member of the ASGCT Communications Committee.
Related Articles