Developing a Gene Therapy for Charcot-Marie-Tooth Disease
November 30, 2022
We talked to Dr. Afrooz Rashnonejad about her experience working to develop a gene therapy for CMT1B and why patient organizations are so important in the process.
 Earlier this year, ASGCT Associate Member Afrooz Rashnonejad, MSc, PhD, received a grant from the Charcot-Marie-Tooth Research Foundation (CMTRF) that will fund her efforts to develop a gene therapy for CMT1B. This is the first-ever gene therapy attempt for this form of the disease.
Earlier this year, ASGCT Associate Member Afrooz Rashnonejad, MSc, PhD, received a grant from the Charcot-Marie-Tooth Research Foundation (CMTRF) that will fund her efforts to develop a gene therapy for CMT1B. This is the first-ever gene therapy attempt for this form of the disease.
We asked Dr. Rashnonejad about her development process so far, challenges she's encountered, and how this gene therapy approach differs from her previous work.
ASGCT: Congratulations on your award! Can you explain what you’ll use it for?
AR: The grant from CMTRF [more than $500,000] will help us initially explore the feasibility of gene therapy in Charcot-Marie-Tooth (CMT1B) mouse models. The knock-down and replacement is a quite novel gene therapy approach, so in this project, we will optimize the approach and investigate the proof-of-principle for gene therapy for CMT1B.
ASGCT: What is CMT1B?
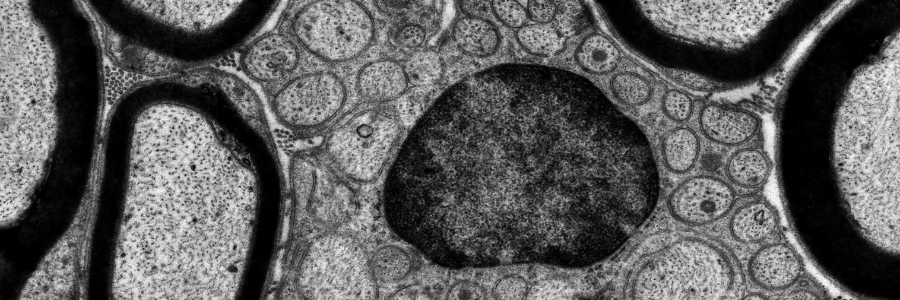
AR:CMT1B arises from numerous different dominant mutations in the myelin protein zero (MPZ) gene that affect Schwann cells (SCs) in the peripheral nerve (PNS). It can be debilitating, with patients showing progressive distal weakness, muscle wasting, sensory loss, and pain. It has two major onsets: infantile (severe, early-onset) and adult (late onset). CMT1B is the second-most common CMT1 neuropathy and is currently untreatable.
ASGCT: What stage are you at in the process of developing a gene therapy for CMT1B? How is this grant going to help move your work forward?
AR: This is a very exciting project and we are at the early stages in the process of developing CMT1B gene therapy. I started running my own lab in April 2022, and, actually, this project is one of the main research topics in my lab. Early funding support we received from the Charcot-Marie-Tooth Research Foundation (CMTR) was essential for our launching the CMT1B program. This is the first-ever gene therapy attempt for CMT1B, and it clearly shows how patient foundations can positively impact research toward therapy development for these patients.
The gene therapy field is advancing rapidly, which paves the way for developing cures for many inherited disorders. We, as scientists, can come up with brilliant ideas to develop a treatment for any disease; however, this isn’t enough because investigating these ideas and translating them to the clinic requires significant capital. Patient foundations have a huge impact on our research and on the field. For example, in our case, CMTRF is the first group that realized the importance of this project, trusted us, provided financial support, and helped us to launch this research to collect proof-of-concept data in a preclinical phase. If successful, it will eventually attract companies that may invest in this program, supporting more expensive parts that require millions of dollars for safety testing in larger animal models that will ensure the treatment is actually safe for humans.
We, as scientists, can come up with brilliant ideas to develop a treatment for any disease; however, this isn’t enough because investigating these ideas and translating them to the clinic requires significant capital.
Afrooz Rashnonejad, MSc, PhD
Moreover, there is an amazing, supportive, and knowledgeable CMT community out there, made of scientists, doctors, and patients who really care and want to find cures for every single form of CMT neuropathies. I’m glad to be part of this family.
ASGCT: What have been some of the most difficult parts of the gene therapy development process so far for this disease?
AR: Each disease, including CMT1B, has its own unique challenges. For example, targeting Schwann cells, the target cells in CMT1B, has been challenging for decades, but now we know that we can deliver genes to these cells. However, if we put the wrong amount of the transgene in the wrong tissues and cells it can cause adverse effects. So, many things can go right or wrong. It’s our responsibility as researchers to understand these challenges and overcome them in the path of therapy development for humans. I’m looking forward to engaging more with the scientific community and establishing collaborations to support the success of this project.
I believe that gene therapy for CMT1B can help treat the disease. We have to apply the lessons we’ve learned from previous gene therapy stories, by designing our experiments better from the beginning and deeply investigating the safety aspects to ensure the translation of our therapies to humans.
ASGCT: How did you begin working on a gene therapy for CMT1B? What interested you about this specific disease?
AR: My interest in science and neurology goes back to my childhood. When I was a very young kid—and at that time there weren’t digital cameras or digital photos—our family had several traditional photo albums that I loved to turn the pages in and ask my parents “who is this?” or “who is that?” There were a few pictures of a very beautiful young lady with my mom who I had never seen before. When I asked my mom who the woman was, she became so emotional and told me the woman was her very close friend. At that age, I didn’t understand why my mom became that emotional or what she was talking about. When I became older, I heard that when my mom was in high school, her close friend died after experiencing sudden neurological symptoms of an unknown (at that time) disease. A year before her death, she experienced pain, fatigue, seizures, dementia, and muscle weakness, and finally became totally bedbound for a few months before losing her life. That loss had a dramatic effect on her family and friends even after many years.
In grad school, I got more curious about genetics and how a small gene mutation can cause devastating diseases, and more importantly, I wanted to know how we could apply technology to prevent or treat genetic diseases. So, I worked on AAV-based in-utero (fetal or prenatal) gene therapy for spinal muscular atrophy, a severe pediatric neurodegenerative disorder. Then, during my postdoc, I continued my studies in the gene therapy field but shifted my focus to RNA silencing strategies, including RNAi and CRISPR-Cas13, for treating facioscapulohumeral muscular dystrophy (FSHD) in Dr. Scott Q. Harper’s lab at Nationwide Children’s Hospital. In the last year of my postdoc, I became familiar with CMT1B neuropathy which causes pain, loss of sensation, and muscle wasting and weakness.
In grad school, I got more curious about genetics and how a small gene mutation can cause devastating diseases, and more importantly, I wanted to know how we could apply technology to prevent or treat genetic diseases.
Afrooz Rashnonejad, MSc, PhD
CMT1B extremely reduces the quality of patients’ lives. It is affecting approximately 1 in 30,000 individuals, which means roughly >10,000 patients in the U.S. that fall under the rare disease definition. But when you look at the entire world this disease affects >260,000 individuals, which is enormous. Patients are suffering from pain, muscle wasting and atrophy, and disfiguring lower limb contractions. In severe forms, the symptoms start off in infancy or childhood and progress to a loss of ambulation by 10 years old. So, reducing the quality of life, in addition to huge healthcare costs, puts pressure on patients, families, and society. There is no cure available for this disease, and I think gene therapy is a rational approach to be applied.
ASGCT: Can you explain how a gene therapy for CMT1B would work, and how it compares to one for FSHD that you have already developed?
Although these two therapies have some similarities, they take two different types of approaches. For FSHD, we needed to completely knock down the expression of the DUX4 gene, because even a very low level of DUX4 protein is highly toxic in muscles and causes muscular dystrophy. I developed RNA-targeting CRISPR-Cas13-mediated and exon-skipping gene therapy approaches for knocking down DUX4 expression. However, for CMT1B, we need to get rid of mutant MPZ expression while maintaining healthy protein expression. So, here we used the “knockdown and replacement” strategy by using miRNA-mediated knockdown of the MPZ and replacing a healthy copy of MPZ cDNA that is resistant to miRNA knockdown, called rMPZ.
Dr. Rashnonejad is an assistant professor and principal investigator in the Abigail Wexner Research Institute at Nationwide Children’s Hospital and in the department of pediatrics at The Ohio State University College of Medicine.
Related Articles