Seeing Ocular Gene Therapy with New Eyes
Karen Bulaklak, Ph.D. - June 03, 2020
Dr. Bulaklak discusses a presentation from the 23rd Annual Meeting about creating gene therapies for the eye.
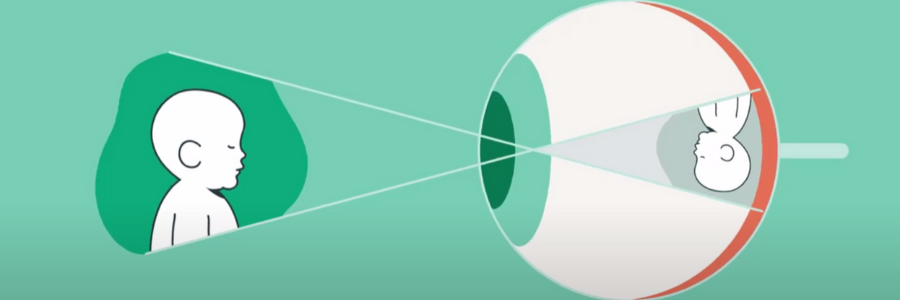
With 21 active clinical trials and approval of Luxturna by the FDA in 2017, the pursuit of gene therapies for ocular diseases is as strong as ever. The eye is a particularly attractive target because of its accessibility, size, and immune privilege. Like Luxturna, many potential therapies currently being studied aim to deliver a transgene for treatment of ocular disease using recombinant AAV vectors. Still, this approach is not one-size-fits-all, and each application comes with its own unique challenges. Local administration via intravitreal or subretinal injection can lead to low target cell transduction or can be procedurally difficult, respectively. AAV vectors also have a small packaging size and may lack the desired cellular tropism. Meanwhile, a large focus has been placed on rare monogenetic disease, which is not representative of the majority of patients in need of ocular therapy. In her talk during the ASGCT 23rd Annual Meeting, “Gene Transfer to the Eye Using Transposons,” Dr. Gabriele Thumann from the University of Geneva spoke about the obstacles in creating gene therapies for the eye and her group’s efforts to overcome them while also reaching a larger patient population.
To address issues with gene delivery, Dr. Thumann first described her approach using transposons. A transposon is a fragment of DNA, such as a therapeutic cassette, that is amenable to being “cut and paste” into the genome with the help of a transposase enzyme. Compared to other non-viral strategies, this technology is highly efficient and allows stable integration. The components can also be delivered ex vivo and in vivo and manufactured using GMP-compliant methods. Dr. Thumann showed how this strategy was under investigation as a potential therapy for neurovascular age-related macular degeneration (nvAMD), which affects a significant portion of the aging population. Anti-VEGF compounds are approved for treatment of nvAMD, but they are costly, have an undesirable pharmacokinetic profile, and require monthly injections into the eye. Dr. Thumann proposed that non-proliferative and non-migrating pigment epithelium (PE) cells can be removed from the patient and electroporated or transfected with a VEGF antagonist, PEDF, along with a transposase. The PE cells are then transplanted back into the eye. The end result would be PE cells that contain a single, stable integration of PEDF, which would act as a depot for secretion of the VEGF antagonist. Preclinical studies in rabbits and rats showed that this therapy was safe, produced significant levels of PEDF and reduced lesion size. One patient has been treated so far and a Phase Ib/IIa for 10 patients has been planned.
As the gene therapy field advances, the goal posts for treatment continue to move to reflect remaining hurdles that hamper efficacy as well as the growing list of indications. Still, groups like Dr. Thumann’s are prepared to take on these challenges in new and creative ways.
Dr. Bulaklak is a member of the ASGCT Communications Committee.
Related Articles