Fauci “Cautiously Optimistic” Regarding a COVID-19 Vaccine This Year
Edith Pfister, Ph.D. - September 15, 2020
Dr. Fauci told attendees he was “cautiously optimistic that we will have an answer by the end of 2020 and we’ll be able to start distributing vaccine in a meaningful way in 2021.”
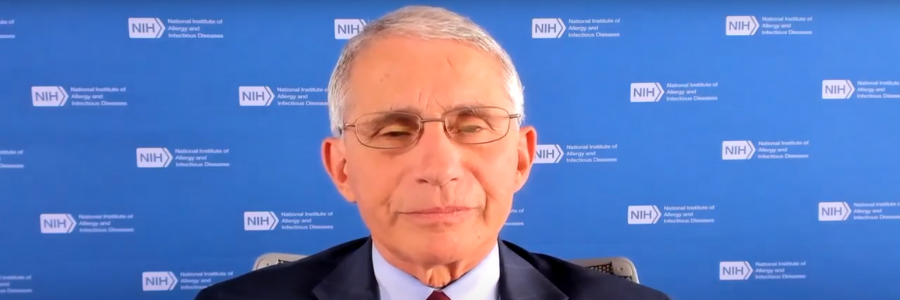
Anthony Fauci, M.D., Director of the National Institute of Allergy and Infectious Diseases kicked off the American Society of Gene & Cell Therapy’s COVID-19 Symposium with a keynote address on Tuesday. In his prerecorded talk, Dr. Fauci told attendees he was “cautiously optimistic that we will have an answer by the end of 2020 and we’ll be able to start distributing vaccine in a meaningful way in 2021.”
Fauci began the talk by providing an overview and context of the COVID-19 pandemic and the SARS-CoV-2 virus.
Development of a vaccine will require unprecedented cooperation. There are seven trials ongoing or planned. The platforms for vaccines generally fall into three categories: nucleic acids, viral vectors and protein subunits. Three trials are in Phase III, and Fauci said he was cautiously optimistic because of favorable data in animal models and in clinical trial results that show the induction of a very good neutralizing antibody response. Although nothing is guaranteed with vaccines, he said, it’s likely we will have some sort of answer between November 2020 and January 2021.
Three types of tests for SARS-CoV-2 exist: molecular tests, which are highly accurate and sensitive, antigen tests to detect the spike protein, and antibody tests. A rapid COVID-19 card test developed by Abbott that costs $5 per test has been purchased by the U.S. government to be used for surveillance.
Treatment guidelines are available at covid19treatmentguidelines.nih.gov and are updated regularly. Drugs under investigation for treatment include monoclonal antibodies and anti-coagulation factors. Hospitalized patients receiving remdesivir exhibit a decrease in time to recovery. Additionally, dexamethasone shows some efficacy for reducing mortality in patients receiving respiratory support.
In December 2019, a novel coronavirus was identified as the cause of a cluster of pneumonia that was sickening workers in a seafood marked in Wuhan, China. Phylogenetically, this coronavirus clusters with the original Severe Acute Respiratory Syndrome (SARS) virus, SARS-CoV, and near to the virus that causes Middle East Respiratory Syndrome (MERS). The disease caused by the virus SARS-CoV-2, COVID-19, has spread around the world in a manner not seen since the 1918 influenza pandemic.
Globally, the virus has infected almost 30 million people and caused almost 900,000 deaths. In the U.S. alone, nearly 6 million people have been infected and there have been close to 190,000 deaths.
In the EU, cases peaked in early March. Since then, infections were brought down through both medical and societal methods, but numbers have recently rebounded as countries reopened.
In contrast, the peak occurred in the U.S. in late March to April, but never returned to an acceptable baseline. Following this, there was an unsuccessful reopening of the economy, particularly in Southern states, and the country continues to add some 40,000-50,000 cases per day. These differences between the U.S. correlate with much greater mobility within the country.
The virus itself is spread by close contact respiratory droplets, including aerosols. It is unclear how much surface contact contributes to the spread. It is found in body fluids, but again, the significance is unclear. It can infect animals, including domesticated animals, but that likely does not contribute to the spread. What is clear is that type and duration of contact are critical to virus spread and can be mitigated by proper use of personal protective equipment, hand washing, masks, and distancing. Infection is most likely to occur in closed setting, such as nursing homes, prisons, and indoor venues with close contact. Approximately 40-45% of infected individuals are asymptomatic and up to 50% of transmission comes from individuals who are asymptomatic. Public health measures to prevent spread include social distancing orders, stay-at-home orders, bans on public gatherings, travel restrictions, aggressive screening and contact tracing.
Symptoms of COVID-19 range from mild to critical. Eighty one percent of cases are mild to moderate, resembling flu, while 14% of cases are severe and 5% are critical. Manifestations of severe disease include acute respiratory distress syndrome, hyperinflammation, acute cardiac or kidney injury, hypercoagulability and in children, a multisystem inflammatory syndrome that resembles Kawasaki syndrome. The fatality rate is variable, ranging from 1-2% to 20%. Risk increases with age and some pre-existing conditions. Finally, there are significant racial and ethnic disparities with Blacks, Hispanics, and Native Americans having a much higher rate of hospitalization than non-Hispanic whites.
Fauci’s presentation led into the first of two full days (September 15-16) of new research and innovative progress from the scientific community fighting both SARS-CoV-2 and COVID-19. All presentations from ASGCT’s COVID-19 Symposium are free to view for the next 30 days by registering online.
Dr. Pfister is assistant professor at the University of Massachusetts Medical School and chair of the ASGCT Communications Committee.
Related Articles