Parkinson’s Disease: Is Gene Therapy the Answer We Have Been Looking For?
Eoghan J. Mulholland, Ph.D. - April 13, 2020
April is Parkinson’s Disease Awareness Month, and here we aim to answer a few burning questions: What is Parkinson’s Disease and does gene therapy offer hope in the treatment of this condition which currently has no cure?
What is Parkinson’s Disease?
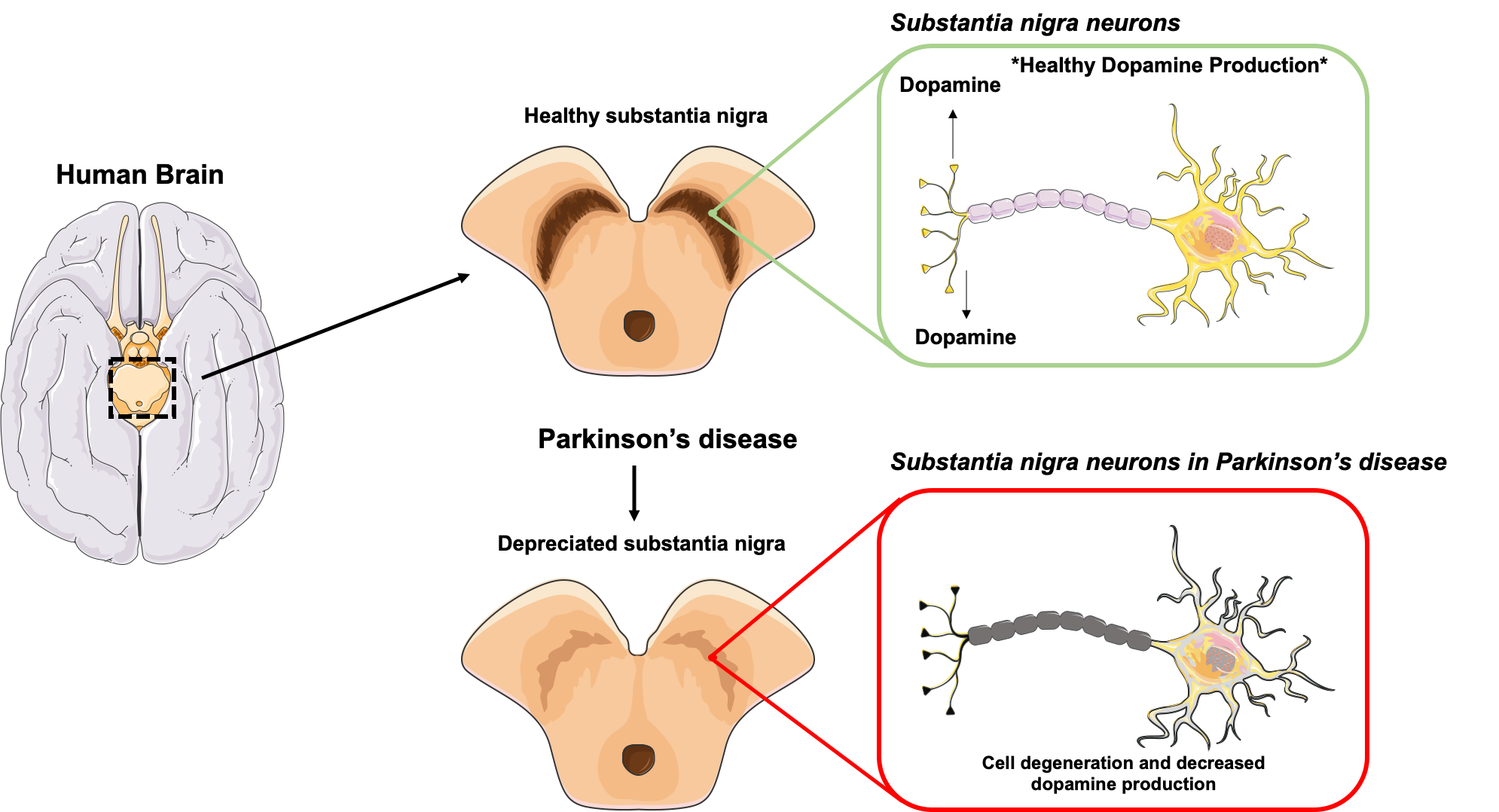
Parkinson’s disease (PD) is a degenerative condition affecting the neurons—nerve cells—in the brain. These cells govern movement through the manufacture of the chemical dopamine. PD is a progressive condition, meaning the symptoms present gradually and slowly worsen. According to the Michael J. Fox Foundation for Parkinson’s Research it is estimated that more than 6 million people have PD worldwide, including 1 million people in the U.S.
Symptoms
PD symptoms vary from patient to patient, with early signs often being mild and often disregarded. When symptoms take hold, they tend to affect one side of the body and gradually worsen on that side, even after both sides become affected. Symptoms of PD according to the Mayo Clinic include:
- Slowed movement. This is also known as bradykinesia and can make simple daily tasks challenging and laborious. Signs of bradykinesia include difficulty getting out of chairs, dragging of feet, and shorter steps when walking.
- Tremor. This symptom typically originates in a hand or finger but can start in any limb.
- Impaired posture. This can present itself as stooped posture and can also lead to balancing problems.
- Impairment or loss of automatic movements. This refers to unconscious movements such as smiling or blinking.
- Rigid muscles. This can occur in any part of the body as muscle stiffness which can be painful and debilitating.
- Speech alternations. Speech can become softer, accelerated, slurred, or even hesitant.
PD diagnosis and current treatments
There is no specific PD test that can be run for diagnosis. Instead PD is diagnosed through a combination of symptom analysis and a neurological and physical examination. Imaging tests which utilize MRI, CT, ultrasound, or PET can be used to help rule out other neurological disorders, but not specifically diagnose PD.
PD does not currently have a cure, but a plethora of medications exist that help to control symptoms. Surgery is also an option, but is typically reserved for advanced cases. The medications offered aim to supplement or increase dopamine to aid in the management of motor problems. Medications can be highly beneficial at the beginning, but the efficacy often drops with time.
Example medications that PD patients may get prescribed include:
Carbidopa-levodopa. Levodopa is noted as the most effective PD medication. It is a chemical that can pass into the brain and convert to dopamine. When combined with carbidopa, levodopa offers protection from early conversion to dopamine outside the brain. This can significantly minimize side effects like nausea. One disadvantage of levodopa is that it can become less potent as the disease progresses.
Dopamine agonists. These therapeutics work to mimic dopamine’s mechanism of action, unlike levodopa which converts to the real thing. Dopamine agonists are not as effective as levodopa in managing the symptoms of PD. However, these drugs have exhibited heightened longevity, so they are often used in in conjunction with levodopa in order to combat its potential loss of potency. Examples of dopamine agonists clinically used include ropinirole and pramipexole, which carry similar side effects to that of levodopa.
Deep brain stimulation (DSB). DSB is a surgical option in which electrodes are implanted into a specific section of a patient’s brain. These electrodes are connected to a generator that is also implanted in the chest area near the patient’s collar bone. This allows for the transmission of electrical pulses to the brain which has been found to reduce the symptoms of PD. The generator can be adjusted post-implantation to personalize the treatment to the patient’s changing disease state. Surgical intervention does come with many associated risks including infection and brain bleeds.
Since PD does not have a cure yet and medication efficacy is variable with time, more effective therapies would be beneficial. Is it possible that gene therapy could be a beacon of hope in this regard?
Gene therapy research
Gene therapy is an exciting option for PD and to date has already shown great potential. Presently, there are 25 trials involving PD and gene therapy listed on clinicaltrials.gov. The overarching goal of gene therapy for PD is to give neural cells the tools to produce dopamine.
Encouragingly there have been many phase 1 clinical trials in recent years that have shown success. For example, in a phase 1 trail sponsored by Genzyme/Voyager, the gene encoding for Aromatic amino acid decarboxylase (AADC) was delivered to the putamen in the brains of PD patients. AADC is an enzyme which is key in the transformation of levodopa to dopamine. The decreasing presence of this AADC enzyme in PD could be linked with the loss of levodopa’s efficiency with time. Thus, increase in AADC expression through gene therapy could result in more effective levodopa treatment. The outcomes of this phase 1 trial were promising in that the patients who received the therapy showed modest improvement in the Unified Parkinson’s Disease Rating Scale and increased FluoroDOPA uptake. The findings of this trial and other gene therapy for PD trials were beautifully summarised in Frontiers in Neuroanatomy.
Of course, the efficiency of any gene therapy is and will be dictated by its mode of packaging and delivery. With delivery of therapeutics to the brain there is also the added hurdle of the blood-brain barrier which restricts drug movement into the brain. I spoke with Dr. Robert M Richardson, who is the director of functional neurosurgery at Massachusetts General Hospital, as well as the Charles A. Pappas Associate Professor in Neurosciences at Harvard Medical School. Richardson and his team have shown fascinating outcomes in the use of MRI-guided convection for enhanced therapeutic delivery. Richardson was also involved in a phase 1 clinical trial of AADC delivery using MRI guided delivery. The findings from this trial were published in 2019 in the Annals of Neurology. Richardson had the following to say:
“The development of iMRI-guided convection-enhanced delivery has established a new era of direct intraparenchymal vector delivery, in which ongoing modification of both individual procedures and overall clinical trial design is imperative for optimizing clinical outcomes.”
The development of processes like this show exciting and novel approaches to the treatment of conditions like PD using gene therapies, as well as other neurological conditions. Please also take the time to read Richardson’s other published work including Gene Therapy for Parkinson's Disease.
Gene therapy has already shown amazing potential in the treatment and management of PD. The current medication and/or surgical options available have varying efficacy with time, and with no cure available action needs to be taken. With advances in therapy delivery to the brain ever evolving there is hope for a new generation of clinically relevant gene therapy options for PD.
Dr. Mulholland is a postdoctoral research scientist in cancer genetics at the University of Oxford and a member of the ASGCT Communications Committee.
Related Articles